 |
          
|
|
Provider Consulting |
"CHC’s contracting efforts and market understanding brought new, immediate, revenue to our organization.” -- Brian Fowler, MD – Urgent Care & Occupational Health Centers of Texas |
|
Managing Your “Managed Care Portfolio” A significant amount of costs, in terms of time and resources, are associated with the effective management of existing and new contractual relationships with third party payers. CHC relieves office staff of the need to managed these contractual relationships and focus on their primary responsibilities. In many cases, this includes: patient care, patient relations, filing of claims, and accounts receivable. CHC’s services ensure best practices are followed, without the need to reinvent existing day-to-day operational workflows, and bring additional revenue opportunities to the organization. (“Contract Cheat Sheet”) |
 |
|
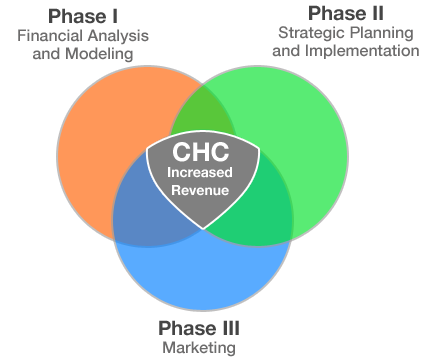
Systematic Approach to Maximizing a Provider’s Profitability Strong, market acceptable, third party payer contracts are integral to the success of any provider practice as they are the primary revenue stream into the organization. Many providers, or provider groups, enter into contractual relationships without fully understanding the nature of their existing patient mix and the complexity behind the third party payer contracts in which they enter. A systematic approach is required to make informed contractual decisions in order to maximize the overall profitability of the organization. CHC has built a reputation to effectively manage these daily administrative tasks while providing long term solutions to the practice. renegotiation efforts patient steerage into “preferred” third party agreements |